A study published in Nature was able to shed light on the changes to the immune system in response to COVID 19 infection. Researchers in Australia were able to get serial blood samples from a patient that was hospitalized with COVID 19 and eventually recovered from the disease.
This is the first study of its kind that has looked at immune-related changes in patients with COVID 19, which provides important insights into the progression of the disease and vaccine development strategies.
The researchers analyzed a number of immune cell subsets over time: Antibody-secreting cells (ASCs), T cell subsets, Natural killer (NK) cells, and monocytes. These cells are important in mounting an anti-viral immune response, and elevated numbers of these cells are observed in patients with Ebola, SARS and H1N1 Influenza infections. Since the data was collected over multiple time-points, it provided a very comprehensive overview of how the immune system in the patient changed over time, from being symptomatic to recovery.
The researchers found that ASCs and a subset of T cells called Follicular T helper cells (TFH) cells were elevated early on in the patient’s blood, but disappeared after recovery. ASCs are key for the rapid production of antibodies following infection with the Ebola virus and vaccination against the influenza virus. and activated circulating TFH cells (cTFH cells) are concomitantly induced following vaccination against the influenza virus. Both these cell subtypes peaked in the blood 3 days before symptom resolution. Activated CD8+ T cells, increased in Ebola and influenza infections, were also increased in this case. Interestingly, there was no increase in circulating NK cells at the time-points assessed. NK cells are the first line of defense against viral infections, whose job is to activate players in the adaptive immune system (viz. CD8 T cells). It is possible that by the time this patient’s blood was evaluated, the NK cells have completed their wave. Blood draw at an earlier time-point would help clarify this point.
What this data means: These results are important for two reasons: 1) These data provide insights on the key immune players mounting an immune response against COVID 19, which might help delineate vaccine development strategies. An ideal vaccine would mimic a natural immune response in order to clear the infection in a short period of time 2) These immune parameters could form crucial diagnostic markers for predicting response to SARS-Cov-2 infection and early identification of people who could recover from the infection.
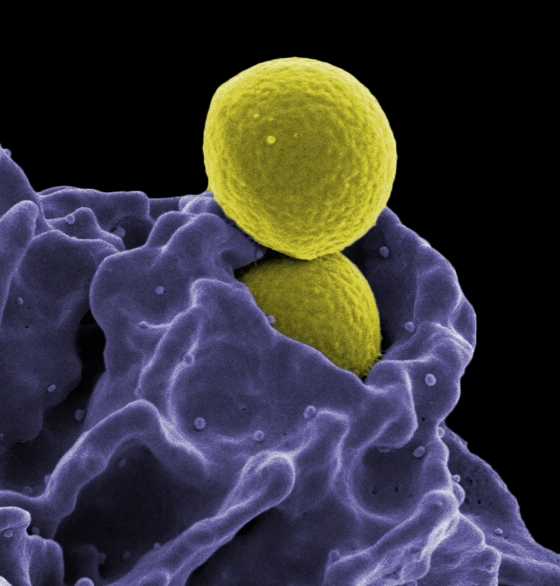
 Photo by
Photo by